Doctors say HCA hospitals push patients into hospice care to improve mortality stats
As Marisol Perez fought for her life in a Texas hospital in autumn 2021, her mother, Alma Salas, sat with her every day praying. Perez, then 42, had such a virulent case of Covid and pneumonia that doctors at St. David’s North Austin Medical Center, an HCA Healthcare facility, had put her on a ventilator and into a coma to try to save her.
Salas said she believed her daughter would pull through, but doctors and nurses at the hospital kept telling her otherwise. Over 10 days in October, less than a month after Perez entered St. David’s, Salas received repeated visits from a palliative care nurse, her hospital record shows. Every other day, Salas said, the nurse urged her to initiate end-of-life care for her daughter. Several of Perez’s doctors also pressed Salas to remove her daughter from the ventilator, she said, in visits confirmed by details from Perez’s chart.
On one occasion, six or seven doctors and nurses gathered around Perez’s bed, Salas said. "We really feel it is in the best interests of your daughter to let her go," she recalled one doctor telling her.
Salas held firm. “I don’t have the authority to take anyone’s life,” she said she told them.
A month later, St. David’s discharged Perez, her chart shows. She went on to make a full recovery.

St. David’s is one of 182 hospitals in the U.S. and the U.K. operated by HCA Healthcare, the nation’s largest hospital chain. HCA is highly profitable — last year it earned $5.6 billion — and its stock is a Wall Street darling.
As an industry leader, HCA’s practices are followed closely by competitors. But HCA’s profits come at a cost to patients and workers, some of its doctors and employees contend. They have cited severe understaffing and insufficient investment in facilities as having caused harm to patients.
Now, new criticisms are arising related to HCA’s palliative and end-of-life care for patients, according to some physicians and nurses who have worked in its facilities. They say HCA officials press staff to persuade families of ailing patients to initiate such care, as Salas says she experienced with her daughter. Although this can harm patients by withdrawing lifesaving treatments, the push can benefit HCA two ways, the doctors and nurses said, and an internal hospital document confirms. It reduces in-hospital mortality rates, a closely watched quality measure, and can free up a hospital bed more quickly for HCA, potentially generating more insurance reimbursements from a new patient.
This article is based on interviews with six nurses and 27 doctors who currently practice at 16 HCA hospitals in seven states or did so previously. All said their HCA hospitals pushed palliative and end-of-life care in pursuit of better performance metrics. Internal HCA hospital documents and texts between hospital staffers provided to NBC News support these health care professionals’ views.
Nurses at HCA hospitals would have owed thousands if they left before 2 years: investigation
May 9, 202304:08Ed Fishbough, an HCA spokesman, denied the contentions. “Suggesting that medical care in HCA Healthcare hospitals is based on anything other than a physician’s independent medical judgment of what is in the patient’s best interest is untrue and wrong,” he said in a statement.
Two weeks after NBC News began raising questions with HCA about its hospice referrals, one physician at a company hospital reported what he believes is a precipitous decline in the number of referrals at the facility.
Regarding Perez’s care at St. David’s, Fishbough said, “Severe, life-threatening illnesses are gut-wrenching experiences, and St. David’s HealthCare physicians, nurses and staff are dedicated to guiding patients and their families throughout the process of managing a severe illness.”
He said he could not discuss details of Perez’s experience because of privacy laws. NBC News provided HCA with a waiver signed by Perez allowing St. David’s Hospital to provide information about her medical care and discuss it with NBC News. HCA said it would only talk about her care if Perez signed two HCA waivers. One was “Authorization for Use and Disclosure of Protected Health Information for Marketing and/or Promotional Purposes” and another was “Consent for Use and Disclosures of Image, Voice and/or Written Testimonials,” giving HCA the right to videotape Perez and record her voice. Perez declined.
Although few patients likely realize it, transfers to hospice care reduce a hospital’s inpatient mortality rate. Here’s why: If a patient passes away in a hospital, that death adds to the facility’s inpatient mortality figures. But if that person dies after a transfer to hospice care — even if the patient stays at the same hospital in the same bed — the death doesn’t count toward the facility’s inpatient mortality rate because the patient was technically discharged from the hospital.
HCA Healthcare low staffing levels accused of endangering patients
Jan. 13, 202303:53A reduction in lengthy patient stays is a second benefit to the push to palliative and then end-of-life care, an HCA hospital document shows. Under end-of-life care, patients don’t typically live long, so the practice can allow HCA to replace patients that may be costing the facility money because their insurance has run out with those who generate fresh revenues.
Offering palliative care to seriously ill patients has gained traction industry-wide in recent years as a treatment for symptoms as well as providing comfort and pain management and support for their families.
Palliative care differs from hospice care. According to the National Institutes of Health, patients in palliative care can receive treatments for symptoms along with those intended to cure their illnesses, while hospice care focuses on comfort and quality of life for a patient approaching death. Patients in hospice typically receive only pain medication, making it crucial, many doctors say, to be cautious when suggesting hospice to family members. Depending on the situation, Medicare, Medicaid and private insurers cover some costs of palliative as well as hospice care.
While palliative care and hospice care differ, the HCA spokesman confirmed that the two treatments work in tandem at its facilities. Palliative care acts as a gateway to hospice care for some patients; if palliative care is recommended, a consultation typically takes place to ensure the patient and family agree. A recommendation to move forward from there to hospice care also requires physician and patient or family sign-off.
For example, one internal HCA document describes palliative care consultations as the first step to hospice care, and another explains how the palliative care coordinator recommends hospice options to family members. If they agree, “the patient will be discharged from an inpatient status and rolled over” into what’s known as General Inpatient Hospice, or GIP, the document says.
An internal HCA hospital analysis from about three years ago shows that almost one-third of its palliative care consultations resulted in admission to inpatient hospice or a hospice discharge plan. Deaths in those plans were excluded from the hospital’s inpatient mortality rate.
Another document recommends palliative care be considered for “patients with prolonged length of stay,” indicating that the services may be seen as a way to reduce patient stays.
At HCA, the push to palliative care and then hospice is constant, according to the doctors and nurses who spoke with NBC News. At two HCA hospitals, the practice appears to be mechanized, with staff citing an algorithm used to identify patients who are most likely to die soon. This is also known as a vulnerability index, texts shared with NBC News show.
Patients ranking high on the vulnerability index become candidates for palliative care, the texts show. In one, a palliative care team member at an HCA hospital identified such a patient; “Algorithm = 97% risk of mortality today,” it said.
The HCA spokesman declined to comment on the algorithm.
One HCA hospital document lists seven ways palliative care helps the facility; topping the list is “Reduction of re-admissions and hospital mortalities that reflect negatively on our hospital.” Another benefit, the document says: “Decrease in hospital length of stay.”
Whistleblower says he's facing retaliation for speaking out about hospital management
Feb. 16, 202305:18Entities rating the quality of care at hospitals track inpatient mortality rates — the popular IBM Watson Health Top Hospitals ranking is an example. HCA’s in-hospital mortality rate is important in another way — it is one of 10 “quality of care” metrics used since 2021 to calculate the incentive pay received by top company executives, its financial filings show. In other words, better mortality results at HCA contributed to better company performance for executive pay purposes.
There is no direct evidence that HCA’s palliative and hospice care push was intended to increase its executives’ pay.
HCA says in its filings that it calculates its mortality rate for pay purposes “internally” using a model devised by IBM Watson Health that excludes patients who die after discharge, such as those in hospice. HCA uses the model “because it includes all patients rather than being limited to Medicare patients, includes more conditions, and has a shorter lag time in the data,” the spokesman said.

Over the two years that HCA’s board has used mortality rates to calculate incentive pay, Samuel N. Hazen, HCA’s chief executive, received $35.3 million in total compensation. Some $305,400 of that was incentive pay generated by the mortality rate calculation, HCA said. Through a spokesman, Hazen declined an interview.
The three major publicly traded hospital companies that HCA considers competitors do not cite the use of mortality rates in their pay calculations, securities filings show. They are Community Health Systems Inc., Tenet Healthcare Corp., and Universal Health Services Inc.
HCA administrators overseeing individual hospitals also receive compensation based on mortality rates, the company said. “We believe all hospital executives should have quality metrics — including mortality — as part of their incentive compensation,” the spokesman said.
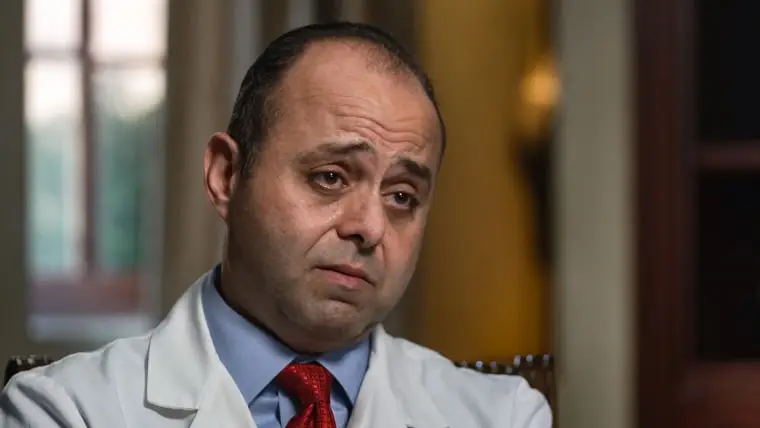
Ghasan Tabel, a doctor who practices at Riverside Community Hospital, an HCA facility in Riverside, California, is troubled by HCA’s palliative care and hospice push. He said he has seen many situations where patients’ families were pressured by staff and told NBC News that the palliative care team does not always consult the attending physician when encouraging a patient’s family to choose the program.
“Sometimes it is reasonable to talk about comfort care, but usually it is done prematurely,” said Tabel, who was involved in a lawsuit against Riverside that the hospital settled. “What is very alarming to me is if they mislead the patient’s family about the prognosis, paint the worst-case scenario, sometimes graphically, to convince the family to go to palliative care and withdrawal of care.”
The HCA spokesman said: “The decision to start palliative care for a patient is based on discussions among the patient, family and physician. Patient care at Riverside Community Hospital is based solely on a physician’s independent medical judgment. Any claims to the contrary are irresponsible and untrue.”
As for Marisol Perez, she believes that if not for her mother, she would be dead and her 9-year-old daughter, Annaliese, orphaned. Of her experience with HCA, she said: “People used as dollar signs and pushed off somewhere else to die — that is not OK.”
'You’re not God'
Tabel is the rare doctor at an HCA hospital voicing public concerns about the company’s palliative care practices. The 26 other doctors NBC News interviewed spoke on the condition of anonymity out of fear of retaliation by the company.
All said, however, that the push for palliative and hospice care at their HCA facilities is insistent and aimed at improving performance measures. Physicians that do not promote the programs are told to toe the line, Tabel and some of the other doctors told NBC News.
One doctor recalled attending meetings at which hospital administrators discussed the importance of transfers to hospice care before a patient dies. “The primary area of discussion was, ‘Why didn’t this patient get moved to hospice 12 hours before?’” the doctor recalled. “'What was the delay in getting them on hospice?’”
Failing to make a well-timed transfer, the doctor said, was considered a “missed hospice opportunity” by the hospital.
HCA declined to comment on this allegation. The company “does not have an enterprise-wide palliative care program,” the spokesman said. “These programs are developed locally under the purview of independent medical staff organizations.”
While the programs may be developed locally, the performance of any hospital deploying them is closely monitored by HCA, a company known for applying performance metrics to all of its facilities and placing them in competition with one another. Speaking at a health care conference last month, Michael A. Marks, senior vice president of finance at HCA, detailed the company’s “internal benchmarking tool that takes 166 measures of cost and operating efficiency” at each facility. “Every hospital will know exactly how they perform against the rest of HCA,” Marks said. “It helps our hospitals really find where their variability is.”
Although HCA does not have an enterprise-wide palliative care program, transfers to hospice care have risen across most of its hospitals in recent years, Medicare claims data shows. Researchers at the Service Employees International Union (SEIU), which has labor agreements with some HCA facilities, found that from 2017 to 2021, the average hospice transfer rate among HCA hospital discharges grew by more than half — from 3.4% to 5.2%.
The national average of hospice transfers also grew during the period, but HCA’s growth rate was roughly double the national average, the research shows.
The research covered 140 hospitals, SEIU said, excluding specialty hospitals like long-term acute care facilities and children’s hospitals, and excluding hospitals with too few claims in a given year. More than half of those hospitals ranked above the 80th percentile nationally for hospice transfer rates in 2021, the analysis shows.
At the same time, in-hospital deaths at the HCA facilities grew far more slowly than the national average, the Medicare data shows. In-hospital deaths at the HCA hospitals rose 17% from 2017 to 2021, while the average rose 45%.
Fishbough, the HCA spokesman, said the company strongly disagrees with the report, calling it inaccurate and misleading. He did not dispute the Medicare data findings in his criticisms.
Maritza Tamarit said she felt pressured to place her disabled husband, Pedro, in hospice care after he’d spent months at HCA Florida Mercy Hospital, a 488-bed acute care facility in Miami, in the summer of 2021.
Pedro Tamarit, 60, entered the hospital in May, with circulation problems in his leg, his wife said. After surgery, his condition worsened.

In September, the push for palliative care began, Tamarit said. “One doctor told me, ‘I think your husband would be better placed in hospice,’” she recalled. “I said, ‘Why?’ and he said, ‘Your husband will not be alive for more than six months.’”
She refused, she said, telling the doctor: “You’re not God to say how long that person can live.”
After Tamarit rejected hospice care for her husband, she took him home, she said. Soon she moved Pedro to a different hospital not owned by HCA. He lived for another year.
“I just wanted my husband to have another chance," Tamarit said. She said she is telling her story so that other people can avoid this experience.
HCA’s spokesman said Mercy Hospital “provides multi-disciplinary patient care, including palliative services, to help patients manage pain and symptoms. As such, care goals are set independently by the treating physicians and care teams in the patient’s best interest.”
'Deceiving changes in mortality reporting'
Academics have begun to notice that transfers of critically ill patients to hospice care can allow hospitals to improve their mortality rates. A study published in the Journal of Healthcare Management in 2020 concluded: “Although appropriate in allowing the positive impact of hospice care,” transfers “may induce deceiving changes in mortality reporting in several high-volume hospital diagnoses.”
Christa Schorr, professor of medicine at Cooper Medical School of Rowan University, in Camden, New Jersey, co-wrote the study. “If you have the capability of providing these services, are you being realistic about what your mortality rate is?” she asked in an interview. Calculating hospital executives’ incentive pay using a mortality rate that can be reduced by hospice transfers “doesn’t seem appropriate,” she added.
HCA neurosurgeon says lives ‘absolutely’ have been lost due to hospital chain’s behavior
Feb. 16, 202304:08Tabel said the palliative and hospice care push at his HCA hospital began in 2019, a time frame supported by documents provided to NBC News and interviews with doctors at other facilities. On Jan. 1 of that year, Hazen became the chief executive of HCA after years in its management ranks. The HCA spokesman declined to say whether Hazen played a role in the heightened focus.
More recent internal documents obtained by NBC News show that an HCA facility closely tracked deaths inside and outside of the palliative care and hospice programs and set goals for deaths in hospice to meet a certain level. When the hospital exceeded the goals — with more deaths occurring in hospice — the facility’s mortality rate dropped.
“Healthcare professionals should present hospice as an option to all patients and families when death within a year would not be surprising and should reintroduce the hospice option as the patient declines,” another HCA hospital document states. It notes that the program was introduced to the hospital’s staff in 2019 and a weekly analysis tracked its progress. Going forward, the document stated, the hospital planned to “offer goals for increased compliance with this standard.”
In addition to being pushed to promote hospice care at Riverside Community Hospital, Tabel says he is pressured to reduce how long his patients remain in the facility. HCA closely monitors a metric known as length-of-stay, internal documents show, and Tabel said he is pressed to discharge patients that he believes are not ready to go.

Limiting lengths of stay at any hospital reduces patients' chance of infection and is a measure of health care efficiency used across the industry. Tabel agrees in concept but says the many elderly and infirm patients he treats require longer stays than the hospital prefers and often have nowhere to go to receive the care they need. He says shorter stays can benefit the hospital by removing a costly patient and freeing up a bed for higher reimbursements.
Tabel said hospital officials have told him they were under pressure from HCA higher-ups and he had to bring his length-of-stay numbers down. Tabel said he told them he would not kick people out of the hospital to improve its numbers.
In 2015 Tabel sued Riverside, alleging retaliation for refusing to meet the hospital’s length-of-stay metric. The hospital reduced patient referrals to him as punishment, he alleged. Riverside disputed his claim, but Tabel received an undisclosed settlement from the hospital in the case in 2019.
Now, Tabel says, the hospital is again pressuring him to reduce his patients’ stays, demanding that he agree to abide by new rules in exchange for keeping his privileges at Riverside. He has refused and his status at the hospital is the subject of an internal hearing.
The HCA spokesman declined to comment, citing the dispute with Tabel, but said that “we hold our independent physicians to high standards on clinical outcomes set by the medical staff.”
Expanding hospice services
Under Medicare rules, when a hospital transfers a patient to hospice care in the same facility, the patient enters what’s called General Inpatient Care, or GIP.
But determining whether a patient is appropriate for GIP requires “careful assessment of pain and other symptoms” that cannot be managed in another setting, the rules say. “GIP is not an ‘automatic’ level of care when a patient is imminently dying,” the National Hospice and Palliative Care Organization says.
One doctor described a procedure at an HCA facility where staff targeted ICU patients for hospice transfers even though they were very near death. The physician said the moves did not benefit the patients and seemed aimed at reducing the hospital’s inpatient mortality rate. The doctor’s experience is supported by the previously cited HCA hospital document detailing the benefits of palliative care to the facility. On the list: “Decrease in futile & high utilization of Emergency Department and ICU.”
HCA’s spokesman declined to comment on the doctor’s allegation. But Medicare data from the SEIU report buttresses the doctor’s concerns.
The researchers tracked how many hospital patients died the same day they were transferred to hospice, a measure of the kind of imminent death cited by the National Hospice and Palliative Care group. At the HCA hospitals, same-day death rates in hospice more than doubled from 2017 to 2021 — rising from 7% to 18%. HCA’s same-day death rates were nearly twice the national average in 2021, the research shows.
Meanwhile, HCA is expanding its hospice services; in 2021, it paid $400 million to acquire a majority stake in the home health and hospice provider Brookdale Healthcare Services. The acquisition added 80 locations and 4,000 staff.